Header Image by © Angelo / Adobe Stock
CoTCCC updates NPA use, let’s break it down thanks to my favorite PJs!
There is limited quality data to suggest that NPA’s are effective in trauma patients (most data is for OSA patients) and a further look shows we may be doing harm with NPAs that are not the right length. US military IFAKs do not match size to the person carrying them, instead it is a one size fits all (with varying sizes depending on where they are sourced from).
This JSOM article from 2021 shows us that our traditional methods of measuring someone for an NPA aren’t accurate. Furthermore, in a study by M.D. Stoneham there is a 7% incidence of moderate to severe bleeding with placement. So maybe it is time to just use a more effective airway measure, the lateral recumbent position (already recommended but often overlooked).
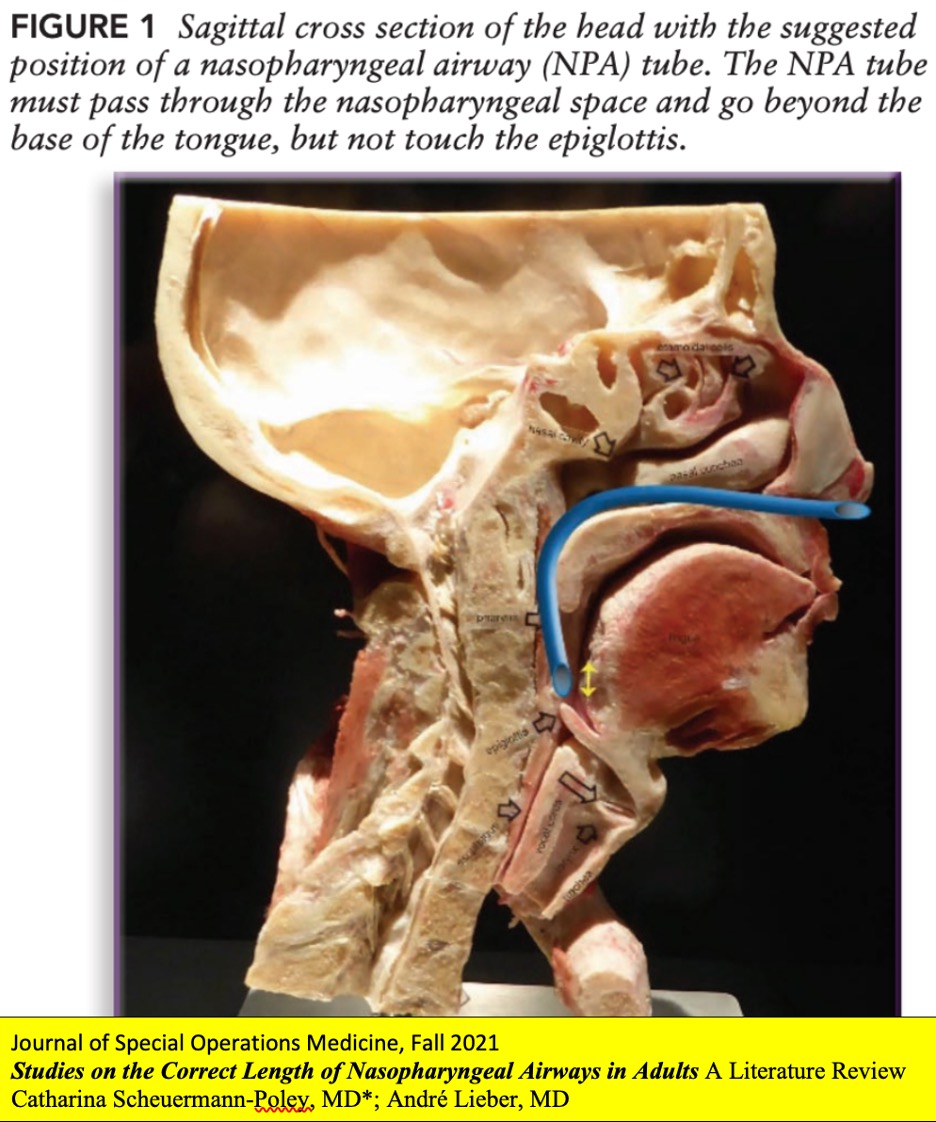
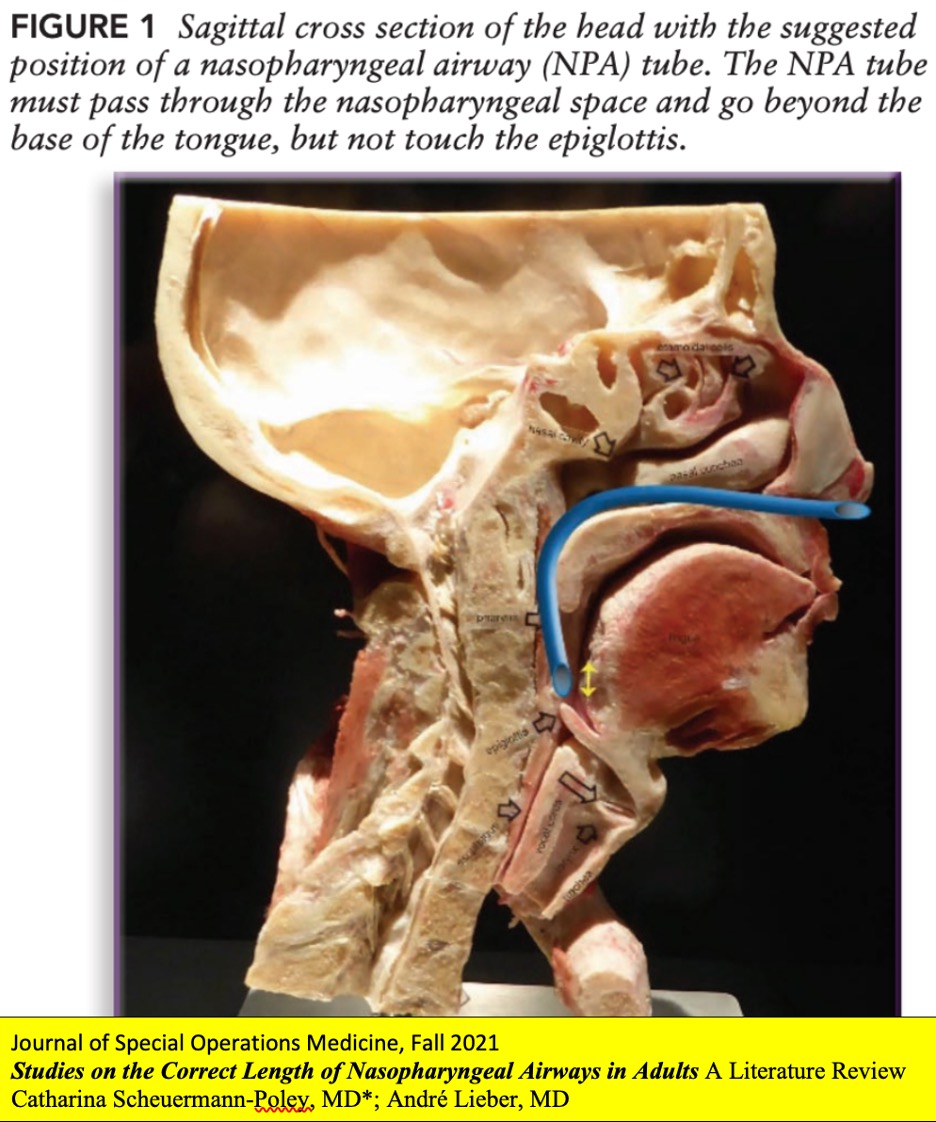
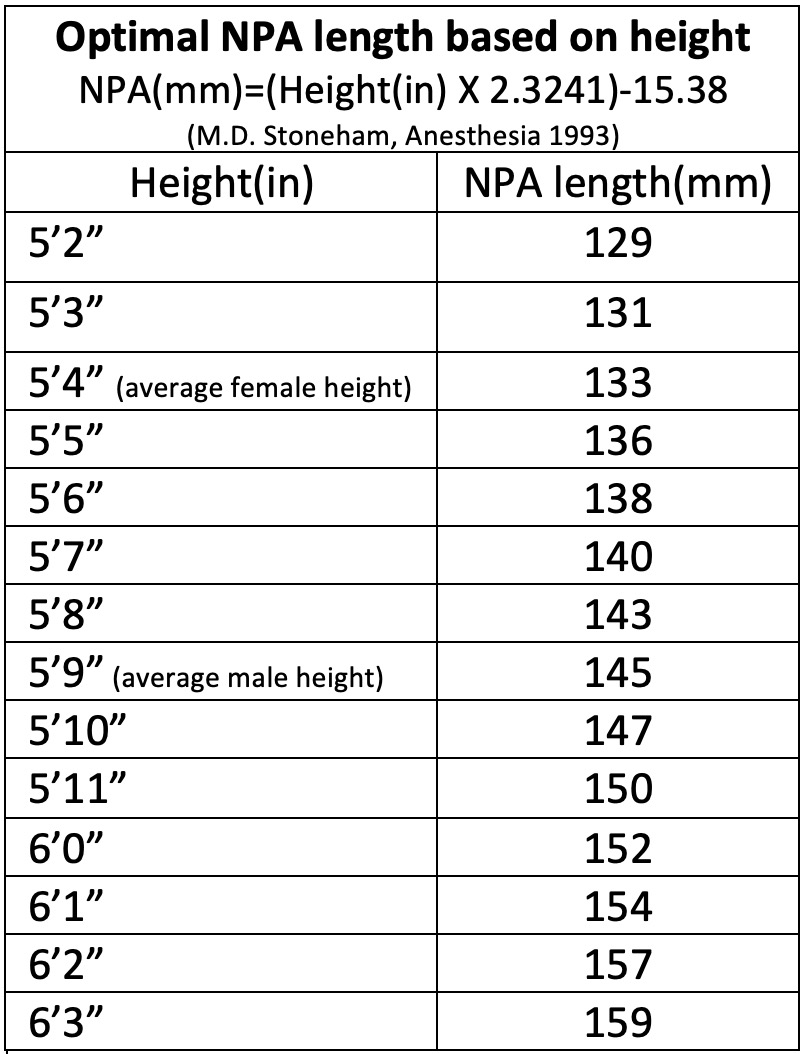
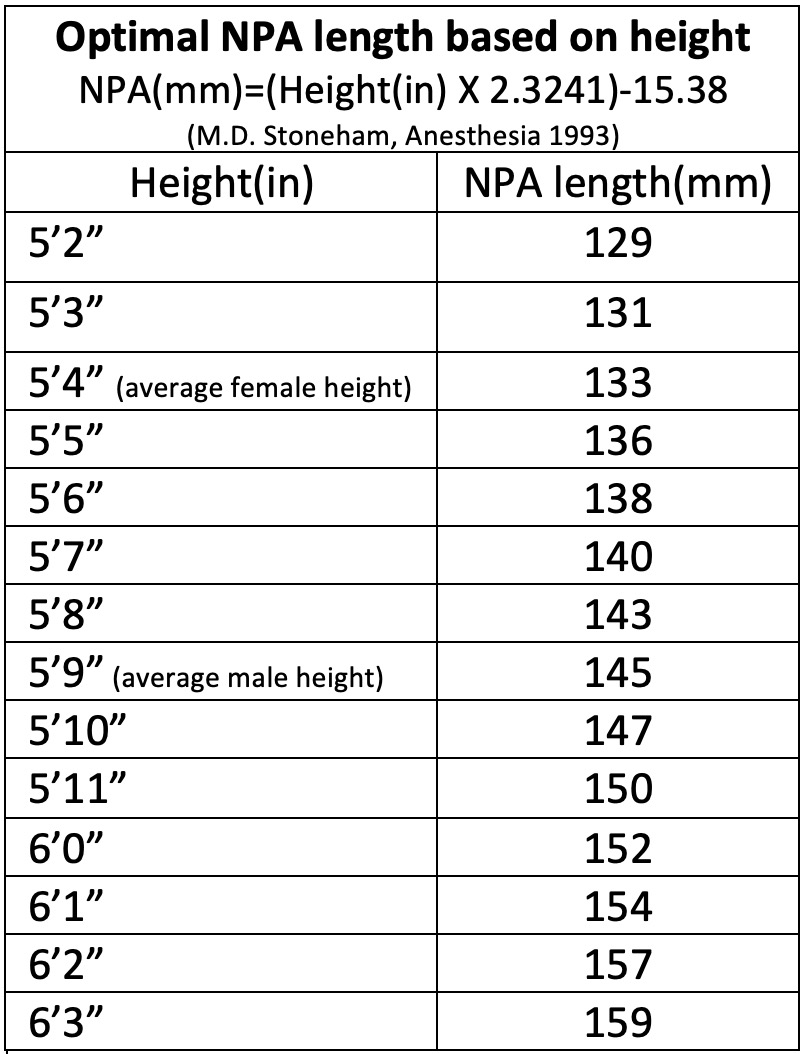
NPA Sizing: Ideal length will have the tip rest 1cm above the epiglottis. NPAs are sold by their French size (French size = 3X OUTER diameter in mm, so a 21 Fr is 7mm diameter). This also means that the French size is approximately the circumference as well. The majority of manufacturers/retailers list the French size and do not include an overall length which makes it difficult to determine if you have the right length. Too short of an NPA and you won’t separate soft palate and tongue, too long and you will gag the patient or hit the esophagus. What is the correct length? NPA Length (mm)= (Height (in) X 2.3241) – 15.38. Try doing that calculation on target!! Next best was the Nares:Tragus length (but it isn’t very accurate). Nares:Epiglottis length was an average 159mm in males, 140mm in females. When you use an average female and male height of 5’4” and 5’9” this gives a size of 133mm for average female and 145mm for average male. If you calculate it out, there is a 30mm size difference between a short female and a tall male, so one size does not fit all!
**NOTE**The above is a breakdown focused on military TC3 use. In other situations (and some military) the NPA can be very beneficial. NPAs can significantly help airflow when using a BVM on your patient. They can also be very beneficial for somnolent patients you may encounter with opiate overdoses as a way to increases airflow temporarily. For a much less useful purpose, training to place these on each other is always a great time! Remember, when placing an NPA, if it causes the patient to cough (touching the epiglottis), then it went too far.



